Jump to the information you need
What is memory?
-
What is memory?
Memory is your brain’s ability to store information and to find it again later. Memory is divided into:
- Short-term memory: deals with information that is only kept for the length of time you need it. For example, remembering a phone number for long enough to dial it
- Long-term memory: deals with any information that is kept for longer than this
“I have found that epilepsy really affects my short-term memory. I can remember things from years ago, but I can’t remember what someone told me five minutes ago.”
Recording the memory in the first place is called encoding. The information is then passed from short-term to long-term memory for storage. You may be better at remembering some things and not others.
“My long term memory is very much affected. Some pretty important events in my life are either completely gone, or I only remember part of them.”
When we want to remember something, the information we need is brought back from long-term memory to short-term memory. This is called retrieval.
If we have forgotten something it could be due to problems with:
- Recording the memory in the first place (encoding)
- The storing of the memory (storage)
- Recovering the memory from long-term memory (retrieval)
-
What causes memory problems?
There is no such thing as “normal memory”. Everyone is different and can have minor lapses in memory from time to time.
Memory loss can be a normal part of getting older. Or it can be caused by some common issues such as:
- Problems with sleep
- Feeling stressed
- Anxiety or depression
But sometimes memory problems can be more severe or last for much longer than normal. Some possible reasons for this include medical conditions like dementia, stroke or epilepsy.
“My memory can be so bad that I might be deep in conversation, stop for one second, and completely forget what I was talking about.”
How and why might epilepsy affect memory?
There are many reasons why people with epilepsy can have problems with memory.
Seizures
Seizures can affect memory because for memory to work properly the brain needs to continuously monitor itself. Epileptic seizures can interfere with this self-monitoring process at any of the following stages:
- Before a seizure: memories from before a seizure can be lost as the brain does not store them properly
- During a seizure: loss of consciousness can stop the brain from recording and storing memories
- After a seizure: confusion can stop memory from working correctly
- Between seizures: Some people with epilepsy may have unusual electrical activity in the brain between seizures. This can affect attention and memory function
“After one of my seizures, I couldn’t remember anything about my life. Then I heard a song from 1996 on the radio – so I started giving hospital staff details about me as if it was that year!”
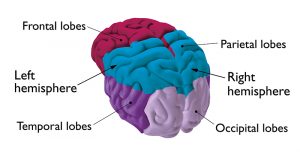
Damage to the temporal lobe
An important part of the brain for storing and recalling information is the temporal lobe. So, if your epilepsy is caused by a problem in the temporal lobe, this can also cause memory problems.
Epilepsy medicine
Epilepsy medicines can have different side effects for different people. Some epilepsy medicines may affect your memory, because they can slow down the speed at which your brain processes information. You may feel drowsy or find it hard to concentrate which can affect how well you store or retrieve information.
On the other hand, epilepsy medicines work to reduce the number of seizures you have. So if you have fewer seizures, this may help your memory.
General wellbeing
Having epilepsy can affect your emotional wellbeing. And this can, in turn, have a big impact on your memory. If you feel stressed, anxious or depressed, you may find it harder to concentrate or think clearly. Or you might pay less attention to what is going on around you.
This makes it harder for you to remember things later. So taking steps to improve your wellbeing can help. We have more information about wellbeing.
Got any questions?
Our expert advisors can help you with any questions you might have about memory or anything else related to living with epilepsy.
Memory problems and work
We hear from lots of people with epilepsy who worry about the impact memory problems have on their work. It can help to talk to your employer and your colleagues about any extra support you might need.
In the UK, if your employer knows about your epilepsy they must make reasonable adjustments to help you do your job. We have more information about reasonable adjustments in our epilepsy and work section.
“When I went back to work I used a diary all the time and had tick-lists, which my colleagues ended up using as well!”
“Setting aside an hour a week to run through next week’s plans works well for me. It doesn’t so much help store and recall ‘when and where’, but it’s a place to look.”
Memory problems and education
Research suggests that over half of children with epilepsy may have problems with memory. If your child has memory problems they may find learning more difficult, and may need extra support at school to help them remember what they are being taught.
If you feel your child may have memory problems you should discuss these issues with the school. We have more information about epilepsy in schools.
If you are in higher education and have memory problems, you could speak to the college or university disability advisor about adjustments to help you. This could include giving you handouts before the lecture, or being given extra time in exams. We have more information about epilepsy in higher education.
“The disability support services at my university provided me with a [device] to record all my lectures. I also would use my phone to record myself, and then right up to an exam I would put my headphones in and listen to myself right up until the exam door.”
“When trying to revise I would really struggle, but I found that associating things with stories and pictures would help. For a tough exam last year I spent a while changing catchy song lyrics to facts and theories and then listened on repeat. It definitely helped!”
Does having epilepsy increase my risk of dementia?
Dementia is the name for a group of symptoms that can affect memory, thinking, language and emotions. It’s a progressive condition, meaning it gets worse over time. It mainly affects people over the age of 65.
Research suggests that people with epilepsy are at greater risk of developing dementia later in life. But the links between epilepsy and dementia aren’t fully understood and it isn’t clear whether epilepsy itself can cause dementia. Instead, the conditions may share common risk factors. For example, if an older person has a stroke, this could increase their risk of both epilepsy and dementia. More research is needed to fully understand the possible links between epilepsy and dementia.
Another possible reason for the link between having epilepsy and developing dementia is that seizures can be a symptom of some types of dementia. For some people, seizures may be one of the first symptoms they or other people notice. If this happens, the person may be diagnosed with epilepsy first, and then diagnosed with dementia later as they start to have other symptoms.
Having memory problems does not necessarily mean you have dementia, or will develop it in later life. But if you’re worried about memory problems or dementia it’s a good idea to speak to your GP, particularly if you’re over 65. They will ask you about your symptoms and health to try to work out the cause of your memory problems.
The NHS website has more information about dementia.
Support for memory problems
There are lots of people who can support you and you do not have to face memory problems on your own. It is ok to ask for help from friends, family or professionals.
If you’re having problems with your memory, it’s a good idea to speak to your GP or epilepsy specialist. They will ask you about your symptoms and health to try to work out the cause of your memory problems.
How are memory problems assessed?
If you are having problems with your memory, your doctor may suggest carrying out a neuropsychological assessment. ‘Neuropsychological’ means looking at the processes that the brain carries out, one of which is memory. This assessment aims to get an accurate idea of how well your memory is working and is carried out by a psychologist.
The assessment will look at your ability to remember pictures, stories and numbers. Through looking at these areas, the psychologist will be able to find out if you have memory problems and where your difficulties lie. They can then suggest what strategies might be most helpful for dealing with your memory problems.
Managing other causes of your memory problems
Your memory problems might be affected by another cause, such as:
- Not getting enough sleep
- Having lots of seizures
- Your epilepsy medicine
- Your mental health, including if you have anxiety or depression
Structured approaches
Your doctor may be able to refer you to a professional that can help with a structured approach such as cognitive rehabilitation. Cognitive rehabilitation focuses on what is important to you and helps you to work on key goals that would make a big difference to your life. Professionals that might offer this include occupational therapists, speech and language therapists and physiotherapists.
It might be possible to make changes to these to help your memory. It’s a good idea to talk to your doctor or epilepsy specialist if you think this applies to you. Epilepsy Action has advice that might be helpful for improving your health and wellbeing.
Managing your memory problems
There are lots of different strategies that might help you to remember things. There may be some ‘trial and error’, until you find the methods that work for you. Some of these methods are:
-
Following a set routine
Following a routine is a good way to help your memory. Having a routine means you can get used to what to expect, which reduces the demands placed on your memory.
A lot of people find it useful to make a note of their regular activities in their diary or on the calendar. Also, always doing things at certain times of the day, for example always taking your medicines with breakfast can help some people.
-
Adapting your surroundings
By making changes to your surroundings you will have less need to use your memory. This can be achieved in a number of ways:
- Keeping a note pad by the phone to take messages
- Using a notice board for important information
- Having a particular place to keep things, such as keys and glasses, and always putting them in the same place
- Labelling cupboards to remind you what goes in them
-
Using memory aids
There is a wide range of external memory aids and the most important thing is to choose something that you feel comfortable with. What suits one person may not necessarily suit another. For example, pictures or diagrams may be more useful for people who find reading difficult.
“I have a notebook with different sections, with lists of various things I’m doing or need to buy, and have a daily ‘things to do’ list.”
-
Possible memory aids
- Mobile phones and apps with alarms and reminders
- Smart technology such as Google Home or Amazon Echo/ Alexa
- Diary/calendar
- Digital voice recorder or tape recorder
- Notebook
- Lists, for example shopping lists
- Alarm clock or timer
- Pill reminder box for medicines
- Post-it notes
- Wall chart or wipe clean memo board
- Photo album or memory book
Support from family and friends
Your family and friends can help you by learning about which strategies you find useful. It’s a good idea to talk to them about your memory problems so that they understand how you feel and how you would like to be supported. For example, do you like people to offer prompts, or do you prefer to just be given more time?
“I have difficulty finding everyday words. I always seem to be apologising and saying ‘that thingy’ or ‘doodah’ to describe what I mean.”
Further information and support
The Alzheimer’s Society have a guide to memory problems with lots of tips and suggestions for managing daily life. Their memory handbook is an excellent resource for both people with and without dementia.
The Children’s Trust has information about memory issues and practical tips to help children with their memory after a brain injury.
NHS Lanarkshire have produced a guide called ‘Practical tips to help my memory’.






