Go straight to the information you need
What are seizure triggers?
Seizure triggers are things that make seizures more likely in people with epilepsy. They’re not usually the same as things that cause, or increase your risk of developing epilepsy.
Most people with epilepsy can identify at least one or two things that trigger their seizures. But not everyone can. And the things that trigger one person’s seizures might not affect someone else in the same way.
The type of epilepsy you have might make a difference to what triggers you have. Some triggers seem to be more common in people who have generalised seizures, and others in people who have focal seizures. Different epilepsy syndromes may also have links with certain triggers. But most of the time, seizure triggers will be very individual to you.
Some people with epilepsy have reflex seizures. These are when you have a seizure every time, or almost every time, you come across a certain trigger. These are a lot less common than other types of triggers.
Here are some of the seizure triggers that have been reported by people with epilepsy:
-
Not taking epilepsy medicine as prescribed
Taking epilepsy medicines regularly, as prescribed by your doctor, will help to keep a steady level of the medicine in your body.
Missing one or more doses of your epilepsy medicine is one of the most common seizure triggers. There can be many reasons for missing medicines. These include forgetting to take it, or not taking it due to the worry of possible side effects. You may be more likely to miss a dose if you’re tired or stressed.
It is important to follow advice from your doctor about how to take your medicine. Sometimes they can interact with other medicines. If you change medicines, there might be different instructions about how to take them.
-
Feeling tired and not sleeping well
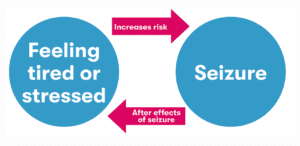
Many people with epilepsy say that feeling tired or not sleeping well can trigger seizures. This can end up causing a cycle, as having seizures can affect your sleep and make you even more tired.
Lack of sleep and tiredness seem to be triggers for both generalised and focal seizures.
-
Stress
It’s not known exactly why stress might trigger seizures. But many people with epilepsy say that if they’re feeling stressed, they are more likely to have a seizure.
For some people, feeling stressed can lead to other changes. This might include feeling anxious or depressed, or changes to your sleeping patterns or eating habits. All of these can also increase your risk of having a seizure.
-
Having an illness which causes a high temperature
Some people report they’re more likely to have seizures when they have a high temperature due to an infection. This can be a particularly common seizure trigger in children. It might be a more common trigger in people who have focal seizures.
We have more information about febrile seizures which are linked with high temperatures, but are not epilepsy.
-
Periods
Some people with epilepsy find that they are more likely to have seizures at certain times of their period (menstrual cycle). There’s some evidence this might be more likely to affect you if you have focal seizures.
Find out more about catamenial epilepsy here.
-
Alcohol
Having one or two drinks from time to time is usually fine for most adults with epilepsy. But drinking larger amounts can increase your risk of having seizures, especially after you stop drinking.
Drinking alcohol can also affect your sleep, and may make you more likely to forget to take your epilepsy medicines. This can also increase your seizure risk.
Find out more about alcohol and epilepsy here.
-
Recreational drugs
Recreational drugs include illegal drugs and ‘legal highs’. There is no control over what goes into these drugs. They can be dangerous and they can trigger seizures. This includes recreational cannabis (marijuana or weed).
Like alcohol, taking cannabis can also make you more likely to have disturbed sleep or miss doses of epilepsy medicine.
This does not include medical cannabis that’s been prescribed by a doctor. Medical cannabis contains pure cannabidiol and can help in some types of epilepsy.
-
Flashing and flickering lights
About 3 to 5 in every 100 people with epilepsy (3-5%) have seizures that are triggered by flashing or flickering lights. This is called photosensitive epilepsy.
If you have photosensitive epilepsy, both natural and artificial light may trigger seizures. This includes light from devices and screens, like TVs, tablets, smartphones and games consoles. You might even find that some patterns, like stripes or checks, trigger seizures.
You would usually have a seizure when you are looking at the trigger, or shortly after.
-
Other possible triggers
There are lots of other factors that people report as possible triggers. A lot of the time, there is little evidence to say for certain whether these things do definitely trigger seizures.
Examples include:
- Exercise – Research suggests that regular exercise can help to reduce your chance of having seizures. Exercise is thought to have benefits for both your body and mind. But there have been some reports of extreme or strenuous exercise causing seizures. It is not clear from the studies whether the exercise caused the seizures
- Missing meals – some people with epilepsy report this as a trigger, but there’s not much evidence to prove a link
- Caffeine in food and drinks – it’s unclear whether caffeine may protect against seizures or make them more likely, due to limited evidence
- Essential oils – these are a form of complementary therapy that some people report as being a trigger
- Smoking and vaping – it’s been suggested that nicotine, or other compounds in cigarette smoke or vape fluids could trigger seizures
- Weather – changes in the weather and extreme temperatures have been reported as seizure triggers, but evidence is mixed
Remember that triggers are different for everyone. Not all of the factors listed above will affect you. What might be a trigger factor for one person may not have any effect on you.
This diagram shows the cycle of having a seizure and being stressed or tired.
How can I recognise my triggers?
Keeping a seizure diary is a good way to try and find out what might trigger your seizures.
Every time you have a seizure, record it and make a note of what you were doing and how you were feeling. If you do this over time, you might see a pattern emerging.
How can I avoid seizure triggers?
It’s not always possible to avoid seizure triggers. Some things may be out of your control, like getting ill with an infection, or your monthly hormone cycle. It’s not always easy to avoid stress or to get enough sleep. But if you know what your triggers are, there may be some things you can do to try and avoid or reduce them. Here are some suggestions:
- Try to get into a routine with taking your epilepsy medicine
- Have a good sleep routine
- Try to reduce any stress
- Limit how much alcohol you drink, and avoid recreational drugs
- Avoid flashing or flickering lights if you have photosensitive epilepsy
- Talk to your doctor if your seizures follow a pattern connected to your periods
Got any questions?
If you have any questions about what might trigger your seizures, or anything else on living with epilepsy, our expert advisors are here to help.
-
Sources
Balamurugan, E. et al. (2013) ‘Perceived trigger factors of seizures in persons with epilepsy’, Seizure, 22(9), pp. 743–747. Available at: https://doi.org/10.1016/j.seizure.2013.05.018
Aldosari, A.N. et al. (2023) ‘The Frequency and Precipitating Factors for Breakthrough Seizures in Children with Epilepsy’ Journal of Epilepsy Research [Preprint]. Available at: https://j-epilepsy.org/journal/view.php?doi=10.14581/jer.23003
Nakken, K.O. et al. (2005) ‘Which seizure-precipitating factors do patients with epilepsy most frequently report?’, Epilepsy & Behavior, 6(1), pp. 85–89. Available at: https://www.epilepsybehavior.com/article/S1525-5050(04)00338-5/abstract
Frucht, M.M, et al. (2000) ‘Distribution of Seizure Precipitants Among Epilepsy Syndromes’ Epilepsia, 41(12), pp. 1534–1539. Available at: https://onlinelibrary.wiley.com/doi/10.1111/j.1499-1654.2000.001534.x
Kasteleijn-Nolst Trenité, D.G.A. (2012) ‘Provoked and reflex seizures: Surprising or common?’, Epilepsia, 53, pp. 105–113. Available at: https://onlinelibrary.wiley.com/doi/10.1111/j.1528-1167.2012.03620.x
vi Legg, K.T. et al. (2017) ‘Counselling adults who experience a first seizure’, Seizure, 49, pp. 64–68. Available at: https://www.seizure-journal.com/article/S1059-1311(16)30161-3/fulltext
Maguire, M.J. and Nevitt, S.J. (2021) ‘Treatments for seizures in catamenial (menstrual-related) epilepsy’, Cochrane Database of Systematic Reviews, 2021(9). Available at: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD013225.pub3/full
Gordon, E. and Devinsky, O. (2001) ‘Alcohol and Marijuana: Effects on Epilepsy and Use by Patients with Epilepsy’, Epilepsia, 42(10), pp. 1266–1272. Available at: https://onlinelibrary.wiley.com/doi/10.1046/j.1528-1157.2001.19301.x
Samsonsen, C. et al. (2018) ‘The seizure precipitating effect of alcohol’, Epilepsy Research, 143, pp. 82–89. Available at: https://www.sciencedirect.com/science/article/abs/pii/S0920121118300378?via%3Dihub
Leach, J.P., Mohanraj, R. and Borland, W. (2012) ‘Alcohol and drugs in epilepsy: Pathophysiology, presentation, possibilities, and prevention’, Epilepsia, 53(s4), pp. 48–57. Available at: https://onlinelibrary.wiley.com/doi/10.1111/j.1528-1167.2012.03613.x
NHS (2022) Medical cannabis (and cannabis oils). Available at: https://www.nhs.uk/conditions/medical-cannabis/ (Accessed 14 December 2023)
NICE British National Formulary (2023) Cannabidiol. Available at: https://bnf.nice.org.uk/drugs/cannabidiol/ (Accessed 14 December 2023)
Shorvon, S. (2010) Handbook of Epilepsy Treatment. 3rd edn. John Wiley & Sons.
Silva, A.M. da and Leal, B. (2017) ‘Photosensitivity and epilepsy: Current concepts and perspectives—A narrative review’, Seizure – European Journal of Epilepsy, 50, pp. 209–218. Available at: https://www.seizure-journal.com/article/S1059-1311(17)30252-2/fulltext
Fisher, R.S. et al. (2022) ‘Visually sensitive seizures: An updated review by the Epilepsy Foundation’, Epilepsia, 63(4), pp. 739–768. Available at: https://onlinelibrary.wiley.com/doi/10.1111/epi.17175
Wilkins, A., Emmett, J. and Harding, G. (2005) ‘Characterizing the Patterned Images That Precipitate Seizures and Optimizing Guidelines To Prevent Them’, Epilepsia, 46(8), pp. 1212–1218. Available at: https://onlinelibrary.wiley.com/doi/10.1111/j.1528-1167.2005.01405.x
Arida, R.M. (2021) ‘Physical exercise and seizure activity’, Biochimica et Biophysica Acta (BBA) – Molecular Basis of Disease, 1867(1), p. 165979. Available at: https://www.sciencedirect.com/science/article/pii/S0925443920303276?via%3Dihub
Duñabeitia, I. et al. (2022) ‘Effects of physical exercise in people with epilepsy: A systematic review and meta-analysis’, Epilepsy & Behavior: E&B, 137(Pt A), p. 108959. Available at: https://www.epilepsybehavior.com/article/S1525-5050(22)00408-5/abstract
Capovilla, G. et al. (2016) ‘Epilepsy, seizures, physical exercise, and sports: A report from the ILAE Task Force on Sports and Epilepsy’, Epilepsia, 57(1), pp. 6–12. Available at: https://onlinelibrary.wiley.com/doi/10.1111/epi.13261
Cavalcante, B.R.R. et al. (2021) ‘Exercise-linked consequences on epilepsy’, Epilepsy & Behavior, 121. Available at: https://www.epilepsybehavior.com/article/S1525-5050(21)00313-9/fulltext
Bauer, P.R. and Sander, J.W. (2019) ‘The Use of Caffeine by People with Epilepsy: the Myths and the Evidence’, Current Neurology and Neuroscience Reports, 19(6). Available at: https://link.springer.com/article/10.1007/s11910-019-0948-5
Bahr, T.A. et al. (2019) ‘The Effects of Various Essential Oils on Epilepsy and Acute Seizure: A Systematic Review’, Evidence-Based Complementary and Alternative Medicine, 2019, pp. 1–14. Available at: https://onlinelibrary.wiley.com/doi/10.1155/2019/6216745
Narrett, J.A. et al. (2023) ‘How do smoking, vaping, and nicotine affect people with epilepsy and seizures? A scoping review protocol’, PLOS ONE, 18(7), pp. e0288120–e0288120. Available at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0288120
Sanja Tomasović et al. (2022) ‘Weather patterns and occurrence of epileptic seizures’, BMC Neurology, 22(1). Available at: https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-021-02535-8
Gulcebi, M.I. et al. (2021) ‘Climate change and epilepsy: Insights from clinical and basic science studies’, Epilepsy & Behavior: E&B, 116, p. 107791. Available at: https://www.epilepsybehavior.com/article/S1525-5050(21)00025-1/abstract
Egenasi, C.K. et al. (2022) ‘Current norms and practices in using a seizure diary for managing epilepsy: A scoping review’, South African Family Practice, 64(1). Available at: https://safpj.co.za/index.php/safpj/article/view/5540