The latest epilepsy news
Who is 2026 Miss GB Surrey contestant Emma Dearling?
Emily Stanley | With Epilepsy Action supporter Emma Dearling beginning a new venture as a contestant on Miss GB Surrey, we share six amazing facts…
The latest epilepsy news
Seven athletes with epilepsy and their stories
Kami Kountcheva | In celebration of the Winter Olympics coming to a close, we spotlight seven athletes with epilepsy and their epilepsy journeys
The latest epilepsy news
PIP assessments leaving claimants with “anxiety” and assessors quitting
Kami Kountcheva | The PIP assessment process is leaving people with epilepsy with “anxiety” and assessors feeling “despised”, while charities urge that the Timms review…
The latest epilepsy news
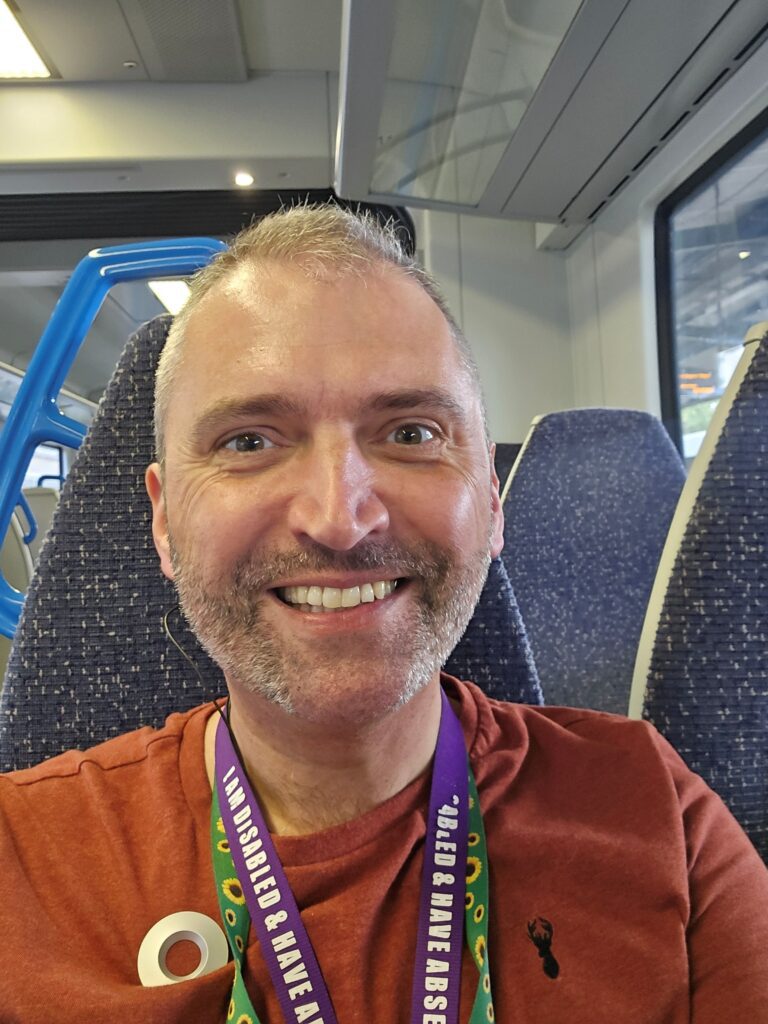
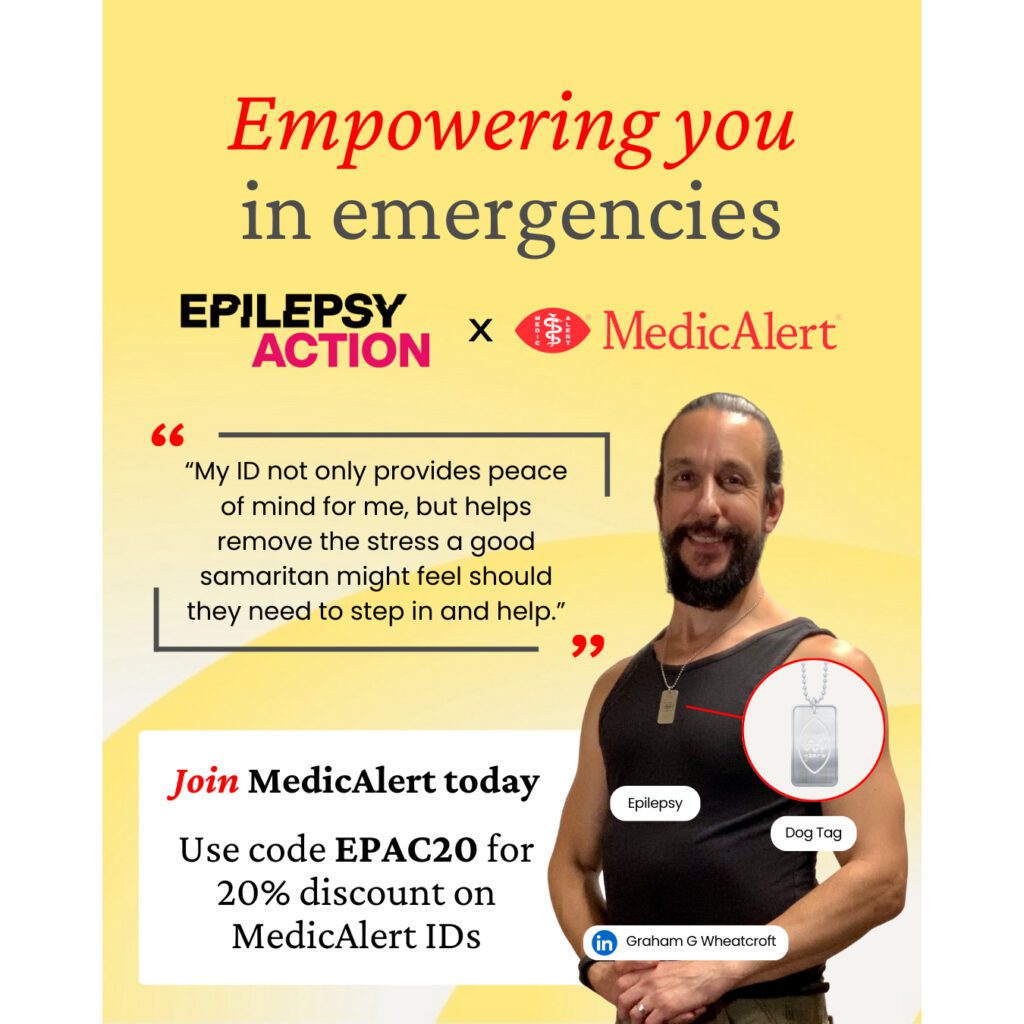
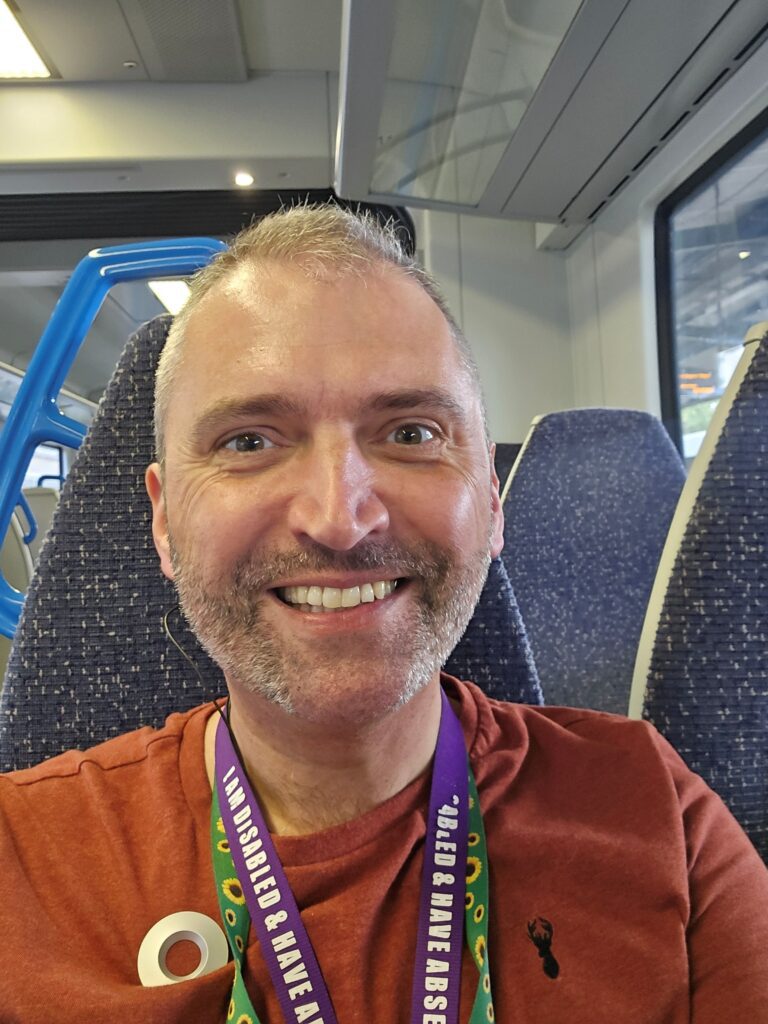
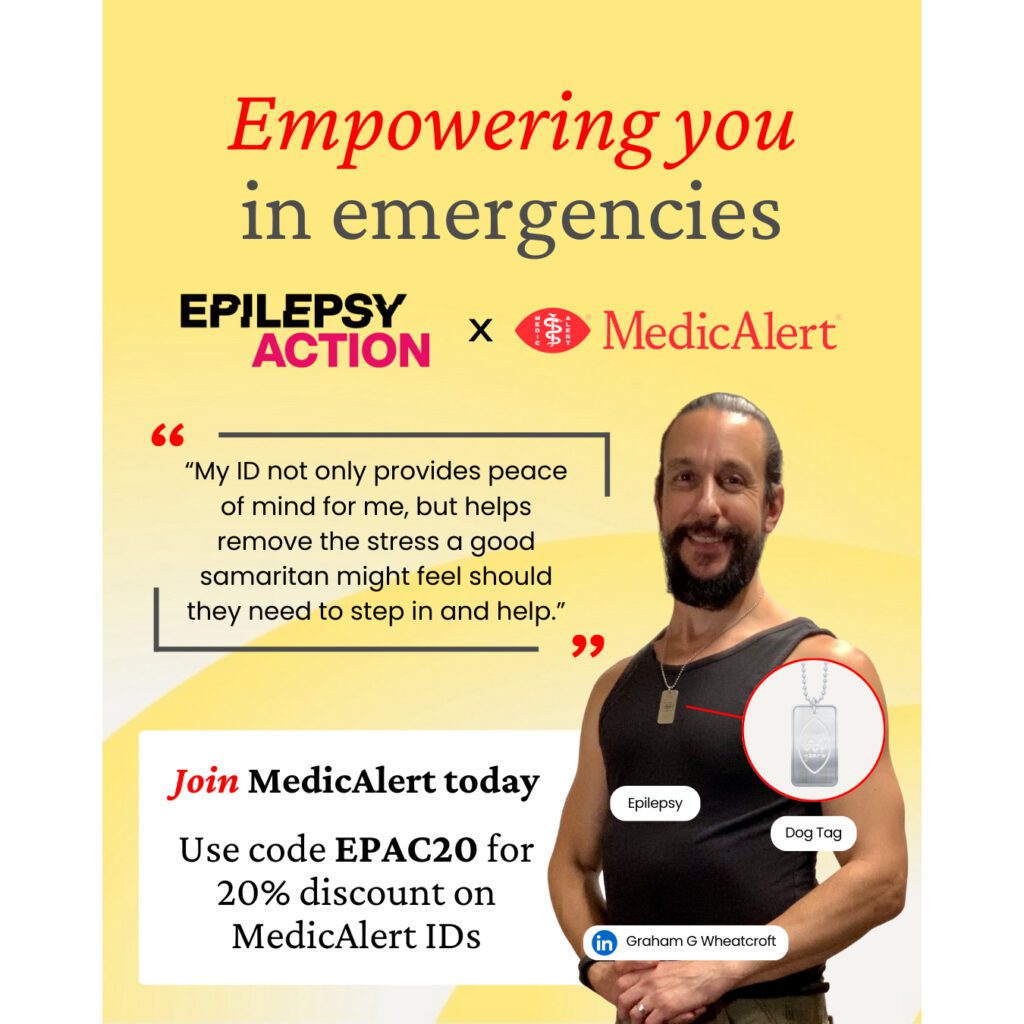
MedicAlert and Epilepsy Action renew partnership to support people living with epilepsy
Epilepsy Action and MedicAlert renew partnership to help bring peace of mind in an emergency to more people with epilepsy
The latest epilepsy news
Valproate scandal compensation: Wes Streeting commits to respond to Hughes Report before next election
Kami Kountcheva | The Health Secretary has said he will respond to recommendations in the Hughes Report into the valproate scandal before the next general…
The latest epilepsy news
Epilepsy on EastEnders: Is Nugget having seizures?
Kami Kountcheva | EastEnders is the latest soap to feature an epilepsy storyline, exploring different types of seizures and their impact on driving
Features
Known risks, no redress: Families still left behind after valproate scandal
Lisa Greer | On the second anniversary of the Hughes report on the valproate scandal, Lorraine’s family, like countless others, is still waiting for essential…
The latest epilepsy news
After the Flood: Epilepsy in hit ITV drama
Kami Kountcheva | After the Flood season two’s central investigation features a character with epilepsy, whose condition is key in unravelling the case. (Beware of…
Purple Day
Fundraise your way and join the Purple Day community
Kami Kountcheva | With Purple Day only weeks away, it’s the perfect time to get inspired by the Purple Day fundraising community and plan your…