Find out more about VNS
How does vagus nerve stimulation therapy work?
The VNS system is made up of 3 parts:
- A small pacemaker-like device, called a generator
- A thin, flexible wire, called a lead
- A hand-held magnet
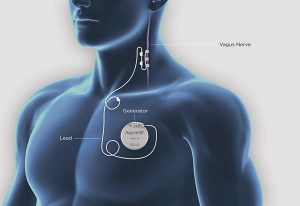
The vagus nerve sends messages between the brain and other parts of the body. In VNS therapy the generator is individually programmed to send electrical pulses to the vagus nerve at regular intervals, all day, every day. These pulses are then carried by the vagus nerve to the brain. This regular stimulation can help to reduce the number of seizures you have and make them less severe.
Newer models of the VNS generator have an AutoStim mode which detects increases in heart-rate. In some people with epilepsy, this can be a sign that they are having a seizure. When the generator detects an increase in heart-rate, it automatically sends an extra dose of therapy to the vagus nerve. This may help to stop a seizure happening or make it less severe.
You can also sweep the hand-held magnet over the generator to send an extra dose of therapy to the vagus nerve. This could be if you feel a seizure starting, or when you are having a seizure. This can stop a seizure happening, shorten the seizure or make the seizure less severe. A carer, or family member, can also use the magnet if they see you having a seizure.
We don’t know exactly how VNS helps to reduce seizures, but research suggests that it may work by:
- Increasing levels of certain brain chemicals called ‘neurotransmitters’
- Increasing blood flow to certain parts of the brain
- Changing patterns of electrical activity in the brain during a seizure
Can I have vagus nerve stimulation therapy?
The National Institute for Health and Care (NICE) guidelines say that VNS therapy may be an option for you if:
- You have drug-resistant epilepsy. This means you have tried 2 or more epilepsy medicines and are still having seizures
- Epilepsy brain surgery is not a suitable option for you
VNS therapy is designed as an add-on treatment alongside epilepsy medicines. It can help to reduce the number of seizures someone has and how severe they are. But it’s not a cure for epilepsy and doesn’t completely stop seizures from happening.
If you think VNS therapy might help you, talk to your epilepsy specialist.
Epilepsy Action has more information about other treatments for epilepsy.
What does VNS surgery involved?
Surgery to implant the VNS system is usually carried out under general anaesthetic. The operation takes between 1 and 2 hours and you can usually go home the same day, or the next day. The procedure involves 2 small cuts, one in a natural crease on the left of your neck, and one in the left-hand side of your chest, below your collarbone. The generator is placed under the skin in your chest. A lead is inserted under the skin to connect the generator to the left vagus nerve in the neck.
As with any operation, there is a slight risk of reaction to the anaesthetic. There is also a small risk of bleeding and infection. Your surgeon will give you more information before the operation takes place.
You might have some pain for a while from the area of the implant after VNS surgery. Your doctor may prescribe medicine to help with this.
What happens after VNS surgery?
The generator is usually left switched off for two weeks after surgery. This is to help your body heal. After that, it is usually switched on by a specialist nurse in a clinic.
How long does the generator last?
At some point, the generator will need replacing when the battery runs low. The generator battery can last between 1 and 16 years, depending on the model and settings used. Your doctor or nurse can tell when the battery is running down during your follow up appointments. They will then arrange for a new generator to be fitted. This involves a small operation, which lasts less than an hour.
How do I get a replacement hand-held magnet?
If you need a replacement hand-held magnet, contact your epilepsy doctor or epilepsy specialist nurse.
What are the benefits and risks of vagus nerve stimulation?
The benefits of VNS can include the following:
- Having fewer seizures – 6 out of 10 people who have VNS fitted find that the number of seizures they have is halved
- Having less severe seizures or shorter seizures
- Better recovery after seizures
- Possibly less epilepsy medicine
- Having improved quality of life
You might find that your seizure control improves slowly over the first 2 years of treatment, rather than straight away.
Risks of VNS:
- VNS therapy is not a cure for epilepsy and it doesn’t work for everyone
- Between 3 and 6 in a 100 people who have had VNS fitted experience infection after surgery. If the infection is minor, this can be treated with antibiotics. But for more serious infection, you may have to have further surgery to remove the VNS device.
Will I still need to take epilepsy medicine after the VNS has been fitted?
VNS is designed to be used in addition to epilepsy medicine, not to replace it. Most people need to keep taking epilepsy medicine after they have had a VNS system fitted. Some people are able to reduce the amount of epilepsy medicine they take over time. You will be able to talk to your epilepsy specialist about any possible changes to your medicine.
Will I get side-effects from VNS?
The most common side-effect reported from VNS is hoarseness or a change in voice. Other common side effects include:
- Sore throat
- Shortness of breath
- Prickling feeling in the skin
- Coughing
Other possible side-effects include changes to heart rate, choking and difficulty swallowing and stomach discomfort. The side-effects of VNS usually happen during stimulation periods, and usually decrease over time. If you find the side-effects uncomfortable, talk to your epilepsy doctor or nurse. They may be able to help by altering the level of stimulation.
You can find a list of possible side-effects in the VNS Patient Manual.
What do I need to be careful about if I have VNS?
MRI scans
If a magnetic resonance imaging (MRI) scan is recommended for you, it’s important that everyone involved in the scan knows about your VNS system. They may need to take precautions to carry out the scan safely. You should have a Patient MRI form from your neurologist to show the people doing the MRI scan.
The VNS Therapy website has a patient MRI form you can download and more information about MRI Safety.
Airport security scanners
Airport security scanners and metal detectors should not cause problems with your VNS. However, the makers of VNS say that to be safe, you should walk through airport scanners at a steady pace, not linger in the area and try to stay at least 40 centimetres away from the equipment. If this is not possible, you could tell the security staff about your VNS and ask for a pat down check instead. Airport staff should avoid using a handheld metal detector directly over your VNS.
Other devices to be aware of
Being close to certain types of equipment can affect your generator:
- You will need advice from your doctor about whether it is safe for you to be where there are pacemaker warning signs. This is because the equipment that could affect a pace-maker could also affect your VNS generator
- Stay at least 60 centimetres (or 2 feet) away from Electronic Article Surveillance System tag deactivators found in shops. This will avoid having your generator activated. These are mostly found in shop entrances
- Tablet computers and their covers, hair clippers, vibrators and loudspeakers can all have electromagnetic field that you need to keep at least 20 centimetres or 8 inches away from your chest. If your generator does become activated, just move away from the device which is causing the problem
You can find a full list of VNS system precautions in the VNS Patient Manual.
Got more questions?
Our expert advisors can help you with any questions you might have about epilepsy treatments or anything else related to living with epilepsy.
How can I find out more?
You can get more information about VNS therapy from the website of LivaNova, who make the VNS therapy system.
Information about vagus nerve stimulation therapy for children
If you’re thinking about VNS therapy for your child, LivaNova have information on their children’s VNS website which may help them understand more. It includes a video you could watch with your child.
This information is currently being reviewed and will be updated soon.





