What would you like to find out about?
Key points
- Where you give birth is your choice
- Your doctor or midwife will encourage you to give birth in hospital so you and your baby can receive emergency care if you have a seizure
- You should continue taking your epilepsy medicines, unless advised by your doctor
- Your doctor or midwife can help you create an epilepsy care plan for you and the birth of your baby
- Most people with epilepsy can have a vaginal birth without complications
- It is rare to have an epileptic seizure during labour
- You will need a review of your epilepsy medicines after giving birth to your baby
- Mental health problems are common during and after pregnancy. There is support available if you need it
Where can I give birth?
You can choose to give birth:
- In a consultant-led maternity unit within a hospital
- In a midwife-led birth unit or centre
- At home
You can base your decision on what your personal preferences are, your health and your baby’s.
The National Institute for Health and Care Excellence (NICE) guidelines recommend that pregnant people with epilepsy give birth in a hospital. This is because you and your baby will have immediate access to emergency care in case you do have a seizure during labour.
If you want to give birth in a stand-alone midwife-led unit or at home, your midwife will arrange for you to speak to a senior midwife. They can help you make sure you have the information you need to make the right choice for you and your baby.
But where you give birth is your decision and your maternity team should support your choice.
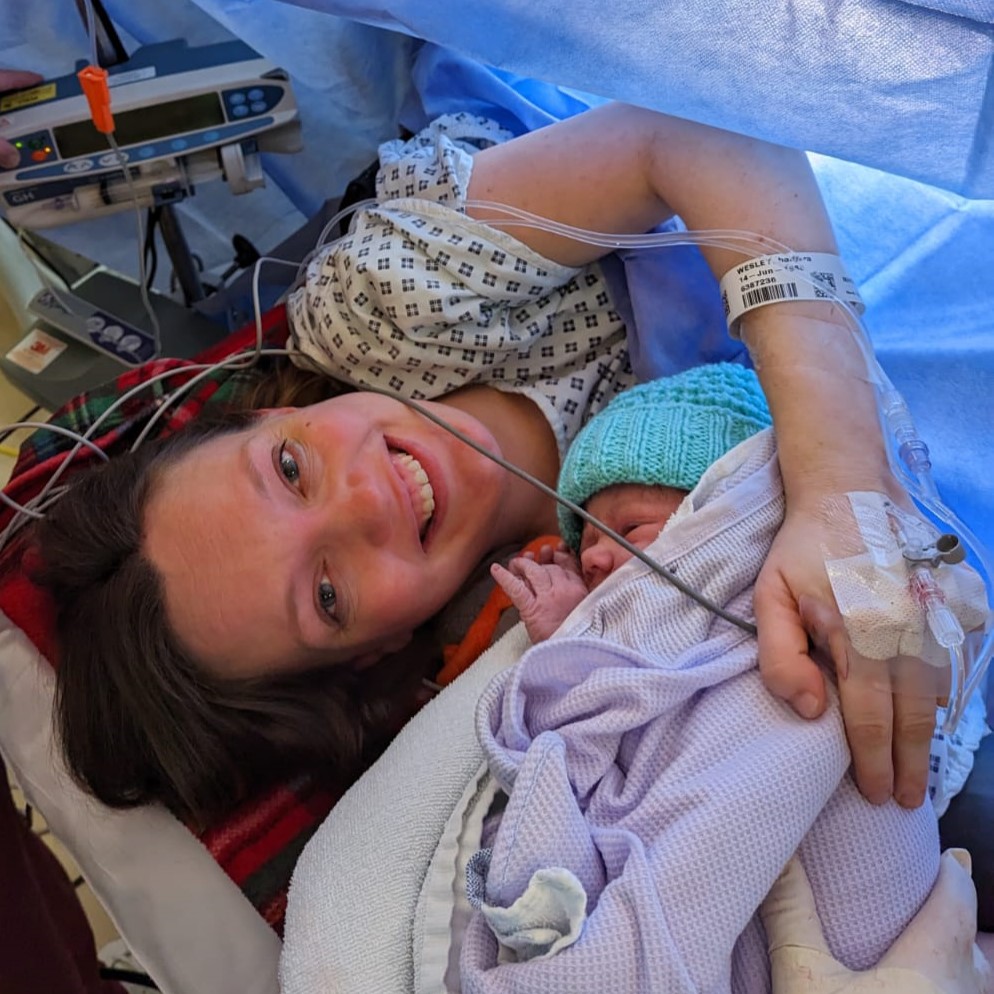
Most people with epilepsy can have a vaginal birth without complications. It is rare to have a seizure during labour.
Your doctor and midwife will talk to you about your options and work with you to complete a risk assessment and make a care plan. They will ask questions about when you last had seizures and if you’re taking epilepsy medicines.
If you are taking epilepsy medicines, you should bring them with you to the hospital when you go into labour and keep taking them as you normally would.
If you stay in hospital at any stage of your pregnancy, you should not stay in a single room on your own. This includes during labour and after the birth. This is to keep you as safe as possible if you have a seizure.
Tip:
If you have decided to give birth at home, make sure you have a supply of your epilepsy medicine packed in a bag. This is so they are ready in case you or your baby need emergency transfer to a hospital.
What pain relief can I have during labour?
There are different options for pain relief during labour.
High doses of the pain relief drug pethidine can trigger seizures in people giving birth with epilepsy. You might be able to have diamorphine instead.
People with epilepsy can:
- Have epidurals (a type of local anaesthetic)
- Have gas and air
You may also be able to use a TENS (transcutaneous electrical nerve stimulation) machine. These are not safe for everyone, so speak to your healthcare professional before using a TENS machine if you have epilepsy. TENS machines are also not recommended early in pregnancy.
Your doctor or midwife can talk to you about the pain relief available and the pros and cons of each. This will help you decide what’s best for you. Just keep in mind that you might change your mind on the day, depending on how your labour progresses and how you feel.
Can I have a water birth?
For most people with epilepsy, using a birthing pool or bath during labour is not safe. This is because of the risk of drowning if you have a seizure.
It might be an option if you have been seizure-free and not taking medicine for a long time. Your midwife or doctor will discuss this with you when you are planning where to have your baby.
Someone should always be with you and there should be a hoist available to get you out of the pool or bath if need be. It’s also important that staff know how to manage a seizure in the water.
Can I have a caesarean section?
A caesarean section, or C-section, is an operation to deliver a baby through a cut made in your tummy and womb.
Epilepsy on its own does not mean you will need a c-section. Your doctor or midwife may talk to you about having a caesarean section if you have regular or long seizures and you are at high risk of status epilepticus.
There may be medical reasons why you will be advised to have a c-section that are not related to epilepsy. Or some people choose to have a caesarean for non-medical reasons.
Your midwife or doctor can talk to you about the risks and benefits of having a caesarean section for you and your baby compared with a vaginal birth.
NHS has more information about caesarean sections.
Supporting someone with epilepsy through labour
There are things you can do to help someone with epilepsy as they give birth. The NHS has some useful general tips and support information for birth partners.
Other advice includes:
- Know what medication the person takes and make sure you have some spare in case they stay in hospital longer than expected
- It is rare for people to have seizures while giving birth. But try to make sure you know what is in the person’s care plan so that you and the medical team know what they want if they have a seizure
- Be prepared to be flexible and supportive if the person changes their mind about what they want at any point during labour
After the birth
-
Vitamin K
Some epilepsy medicines can lower your baby’s vitamin K levels.
You’ll be offered a vitamin K injection for your baby soon after giving birth.
Everyone who gives birth is offered this injection. It helps prevent a rare bleeding disorder called haemorrhagic disease of the newborn.
-
Can I breastfeed?
How you choose to feed your baby is a very personal decision.
If you want to breastfeed, there is usually no reason why you can’t do this. Some people worry about epilepsy medicines being passed on to their baby through breastmilk. But evidence shows that most people with epilepsy taking commonly used epilepsy medicines can breastfeed safely.
Talk to a midwife, infant feeding advisor or your doctor about breastfeeding during your pregnancy. This will help you feel prepared.
The advice they give will depend on:
- The epilepsy medicine you are taking
- The type of seizures you have
- Whether your baby is likely to be born before 37 weeks of pregnancy (premature)
- Your baby’s health
Side effects
Side effects from epilepsy medicines in breastfed babies are rare.
These side effects may depend on what epilepsy medicines you are taking. But they can include:
- Drowsiness
- Poor feeding
- Reduced weight gain
Speak to your midwife, health visitor or GP as soon as you can if you have any concerns.
Call 999 if your baby:
- Does not respond to you
- Is increasingly sleepy
- Hard to wake
- Has difficulty breathing
You know your baby, so trust your instincts. If you think something is seriously wrong, do not hesitate to get medical help straight away.
Rashes in babies
Many things can cause a rash in babies and they are often nothing to worry about.
A rash can also be a side effect of epilepsy medicine in breastmilk. Call your GP or NHS 111 if you are concerned about your baby’s rash.
Call 999 if your baby has a rash and seems seriously unwell. NHS has more information about rashes in babies and children.
Other feeding options
If you do not want to breastfeed or are unable to, there are other options. These include formula feeding or a combination of breastfeeding and formula feeds.
NHS has more information about feeding your baby and Epilepsy Action has some safety tips about it.
-
Lack of sleep
Your baby will have their own pattern of waking and sleeping, which is unlikely to fit with yours. So your sleep may be poor for a while. This may cause problems if lack of sleep is a trigger for your seizures. It may help to:
- Talk to your health visitor about how you and your baby are sleeping. They may have some tips and advice
- Follow safer sleeping advice. The Lullaby Trust has more information about safe sleep for babies
- Ask others for help. If you have a partner, they may be able to feed your baby with expressed or formula milk during the night
- Create a soothing bedtime routine. You may need to tweak your own bedtime routine to make sure you get a good night’s sleep. This may mean going to bed early and at the same time every night for a while
The NHS website has some useful information about helping your baby to sleep.
-
Co-sleeping
It’s best not to share a bed with your baby or young child if you have epilepsy. There is a chance the child may be injured if you have a seizure while co-sleeping, or take medication that causes drowsiness.
All new parents are advised not to fall asleep with their baby on a sofa or armchair.
The safest place for your baby to sleep for the first 6 months is in their cot, lying on their back, in the same room as you.
-
Do I need my epilepsy medicines adjusting after the birth?
If your epilepsy medicine increased while you were pregnant, it may need re-assessing once your baby is born. Otherwise, you might get side effects from taking too much. You may need to have your medicines reviewed before you go home, if you’re in hospital.
It’s worth talking with your doctor or epilepsy nurse about this and having a plan in place before you go into labour. You can use page 4 of the epilepsy maternity toolkit to do this.
Support for you
It can sometimes help to talk to other people going through something similar. We have a talk and support group for parents with epilepsy.
Your mental health after giving birth
Many people find it hard to talk about negative feelings after having a baby. But having a baby is a huge life change and there is no need to feel guilty. Mental health problems are very common during and after pregnancy.
Postnatal depression
It’s usual to feel a bit down, tearful or anxious in the first week or two after having a baby. This doesn’t usually last more than two weeks. But if it does, it could be postnatal depression (PND).
Some studies suggest that people with epilepsy have a high risk of PND. Talk to your health visitor or doctor if you have symptoms of PND. They will be able to help you.
Anyone can get PND and it is important to remember that it is not your fault.
A doctor may prescribe anti-depressants. This is very unlikely to make your seizures worse. Most people who take anti-depressants should still be able to breastfeed. If you have concerns speak to the doctor who prescribed them.
The Royal College of Psychiatrists’ website has more information about post-natal depression and support for postnatal depression.
We have more information about depression and epilepsy.
Anxiety
Anxiety is a feeling of unease, worry or fear. This can be mild or severe. Many parents with epilepsy will have anxiety. This might be due to worries about having seizures while caring for a child, or the side effects of medication. There are steps you can take to reduce any safety risk to you and your baby. Speak to your health visitor or GP if your anxiety starts to get in the way of your everyday life.
Treatment for anxiety may include talking therapies and medication.
We have more information about anxiety and epilepsy.
Looking after yourself and your baby
Caring for a baby is hard work and all parents need help from time to time. If you are still having seizures, it can be even more of a challenge. You might need to put extra safety measures in place. This will also depend on what kind of seizures you have. Remember it is okay to ask for help when you need it.
It can be hard to remember to take care of yourself when you have a baby. You are likely to have more disturbed sleep and you might be more forgetful. This is natural. Missing medication and lack of sleep are common triggers for seizures. It’s important to plan ahead and do what you can to reduce your risk.
If you notice changes in your seizure control after you’ve had your baby, talk to your doctor or epilepsy nurse.
For more information, see our tips for looking after a baby or young child when you have epilepsy.
More information and support
The Royal College of Obstetricians and Gynaecologists
RCOG has useful patient information on their website.
Antenatal Results and Choices (ARC)
Provides impartial information and support for before, during and after antenatal screening.
Provides Information, advice and sources of support for labour and birth
Provides information about keeping well after having a baby and where to get support.
Keeping pregnancy safe
Most people with epilepsy have safe pregnancies and healthy babies. But we know that people with epilepsy can face specific challenges during pregnancy.
This is why we’re working with the maternity and midwifery team covering the North West of England to identify some of these issues and improve outcomes and experiences during pregnancy.